Vitamin D
Firstly, Vitamin D is not actually a vitamin but a hormone! However for simplicity we will refer to it as Vitamin D throughout this post.
Why Do We Need It?
Imagine your body is a well-oiled machine, constantly working behind the scenes to keep you healthy and strong. One of the essential ingredients this machine needs to function properly is vitamin D. Often nicknamed the “sunshine vitamin,” vitamin D plays a much bigger role than just preventing rickets, the childhood bone disease most of us associate with it.
Think of vitamin D as the conductor of a massive orchestra. It helps different parts of your body communicate and work together seamlessly. From your bones and muscles to your immune system and even your mood, vitamin D keeps the music playing in perfect harmony. But just like a dusty record player, if your vitamin D levels are low, the music starts to sputter and stall. This can lead to a cascade of health problems you might not even associate with a lack of sunshine.
So, buckle up and get ready to learn why vitamin D is more than just a beach bum’s best friend. It’s a vital nutrient that plays a starring role in your overall health and well-being.
Can we make Vitamin D?
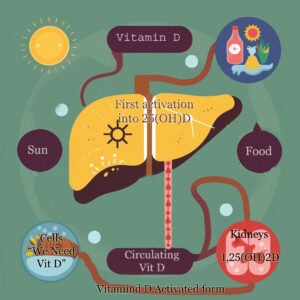
Our bodies can actually make vitamin D on their own, but they need a little help from the sun. When ultraviolet B (UVB) rays from sunlight hit our skin, they interact with a molecule called 7-dehydrocholesterol – let’s call it 7-DHC, naturally present in our skin cells.
7-DHC acts like a light-activated switch in the skin, kickstarting the vitamin D production process once it absorbs UVB rays
This triggers a chemical reaction that converts 7-DHC into pre-vitamin D3. This pre-vitamin D3 needs additional sunlight exposure or body heat to complete its conversion into the usable form, vitamin D3.
Once pre- vitamin D3 is produced in the skin, it enters the bloodstream through tiny blood vessels.
From there, it hitches a ride on protein carriers that transport it to the liver, the body’s processing center.
In the liver, pre-vitamin D3 undergoes its first activation into 25-hydroxyvitamin D (25(OH)D). This 25(OH)D is the form most often measured in a blood test to assess vitamin D status.
At this point the 25(OH)D is considered the “storage” form and can be stored in the blood for weeks, even months. When the body (i.e. cells) require vitamin D3, it will be sent to the Kidneys for final activation into 1,25-dihydroxyvitamin D (1,25(OH)2D). This active form can then bind to receptors in cells throughout the body, influencing various physiological processes.

How long does it take to make Vitamin D?
The process of vitamin D production from sun exposure to reaching the bloodstream is estimated to take between 48-72 hours.
Timeline Breakdown
- Exposure to UVB rays: This happens within minutes of sunlight hitting your skin.
- Conversion to pre-vitamin D3: This initial conversion occurs within a few hours in the skin.
- Conversion to vitamin D3: This final stage, requiring additional sunlight or body heat, can take 24-48 hours and happens in the skin.
- Entry into bloodstream: Once vitamin D3 is produced in the skin, it enters the bloodstream through capillaries within minutes to hours.
- Liver activation: After entering the bloodstream, vitamin D3 travels to the liver where it undergoes its first activation into 25-hydroxyvitamin D (25(OH)D). This process typically takes a few days. This 25(OH)D is the form most often measured in a blood test to assess vitamin D status. It’s considered a storage form because it can circulate in the blood for weeks or even months.
- Kidney Activation: When the body needs Vitamin D for various functions, the 25(OH)D travels to the kidneys. Here, the kidneys perform the final activation step, converting 25(OH)D into the most active form, 1,25-dihydroxyvitamin D (1,25(OH)2D).
Measuring Blood Levels of Vitamin D3
The amount of vitamin D3 in your blood is typically measured in two main units:
- Nanograms per Milliliter (ng/mL): This is the most common unit used for reporting vitamin D levels in blood tests. It represents the weight (nanograms) of vitamin D3 per unit volume (milliliter) of your blood.
- Nanomoles per Liter (nmol/L): This unit is also used in some countries and by some laboratories. It expresses the amount of vitamin D3 based on moles (a unit of measurement for the amount of a substance) per liter of your blood.
While both units represent vitamin D3 concentration, they are not directly interchangeable. Here’s a conversion factor to help you navigate between them:
- 1 nmol/L is equivalent to 2.5 ng/mL
Interpreting Your Results
The optimal range for vitamin D3 levels can vary depending on the laboratory and healthcare professional interpreting your results. However, a general guideline is:
- Deficiency: Less than 20 ng/mL (or 50 nmol/L)
- Insufficiency: 20-30 ng/mL (or 50-75 nmol/L)
- Optimal: 50-100 ng/mL (or 125-250 nmol/L)
- Toxicity: Greater than 100 ng/mL (or 250 nmol/L) (Toxicity from vitamin D is rare)
Supplements: Demystifying Measurements: IU, mcg, and mg
Understanding vitamin D levels and recommendations can be confusing with all the different units thrown around.
Dr. Grimes uses a mouse analogy to explain vitamin D recommendations.
Vitamin D cannot be directly measured by weight, so its potency was based on biological effects. One unit of vitamin D was defined as the amount needed to meet the daily requirement of a 10-gram mouse.
Extrapolating this to a 60kg human would suggest a starting point of 6,000 IU. Dr. Grimes proposes a more personalized approach, similar to how insulin medication is adjusted. This would involve starting with a moderate dose (e.g., 3,000 IU), monitoring vitamin D levels through blood tests, and adjusting the dosage until optimal levels are reached.
Let’s break down what these terms mean and how they relate to vitamin D:
1. International Units (IU):
- This is the most common unit used for measuring vitamin D in supplements and dietary recommendations.
- Think of it like a unit for “vitamin D potency.”
- One IU roughly corresponds to the biological activity of 0.025 micrograms of cholecalciferol (vitamin D3), the most common form of vitamin D.
2. Milligrams (mg):
- This is a unit of mass equal to one-thousandth of a gram (1 mg = 0.001 g).
- It’s a larger unit of mass compared to mcg and is rarely used for vitamin D specifically.
You might see it used for other vitamins or minerals with higher dosages.
3. Micrograms (mcg):
- This is a unit of mass equal to one-millionth of a gram (1 mcg = 0.000 001 g).
- It’s a more precise way to measure the actual weight of vitamin D.
- Some countries, like Canada, use mcg for vitamin D labeling on supplements and blood test results.
Here’s a conversion table to help you compare these units:
| Unit | Equivalent |
| 1 IU | Approximately 0.025 mcg |
| 1 mcg | 40 IU |
| 1 mg | 40,000 IU |
Understanding Vitamin D Levels and Daily Needs
The 400 IU Debate: Rickets Prevention vs. Optimal Health
The current recommendation of 400 IU (International Units) of vitamin D per day is often a topic of debate, particularly in light of Dr. Grimes’ discussion. While this level may be sufficient to prevent the classic childhood bone disease rickets, emerging research suggests it might not be enough for optimal health across the population.
Here’s a breakdown of the issue:
- Rickets Prevention: The 400 IU recommendation originated from historical studies focused on preventing rickets. This level was found to be effective in preventing the severe bone deformities associated with the disease.
- Beyond Rickets: However, Dr. Grimes highlights the broader role vitamin D plays in the body. New research suggests vitamin D benefits extend beyond bone health, potentially impacting the immune system, mood regulation, and even cell growth.
Rethinking Our Needs in a Modern World
Sunshine on Lockdown: Our modern lifestyles often confine us indoors for work, school, and entertainment. This significantly reduces our exposure to sunlight, the natural trigger for vitamin D production in our bodies. Compared to our sun-drenched ancestors, we spend a fraction of the time outdoors, potentially leading to widespread vitamin D deficiency.
Skin Tone Matters: Melanin, the pigment that gives skin its color, also affects vitamin D production. People with darker skin tones naturally produce less vitamin D from sunlight compared to those with lighter skin. This becomes even more critical for ethnic minorities living in northern hemisphere regions with less sunshine exposure throughout the year. They face a double whammy – limited sun exposure and reduced natural production due to skin pigmentation.
Beyond Sunshine: Even with adequate sun exposure, some individuals might struggle to achieve optimal vitamin D levels. Here’s why:
- Body Weight: Obesity can be another factor limiting vitamin D production. Vitamin D is a fat-soluble vitamin, meaning it gets stored in fat tissue. In obese individuals, this storage effect can make it less available for circulation in the bloodstream, potentially leading to lower levels despite sufficient sun exposure and/or supplementation.
The result? Many people, particularly those with limited sun exposure, darker skin tones, or obesity, might not be getting enough vitamin D from sunlight alone to reach optimal levels.
Sunshine or Supplement: Understanding Vitamin D Sources
Dietary sources like fatty fish and eggs can contribute a small amount, but these aren’t always enough to reach optimal levels. This is where vitamin D supplements come in. These supplements typically contain vitamin D3, the form our bodies naturally produce from sunlight. Once ingested, vitamin D3 travels to the liver where it undergoes its first activation into 25-hydroxyvitamin D (25(OH)D). This is the form most often measured in a blood test to assess vitamin D status.
However, there’s another player in the game: calcifediol. This is the already-activated form of vitamin D, ready for the kidneys to convert it into its final usable form, 1,25-dihydroxyvitamin D (1,25(OH)2D). Calcifediol supplements can be helpful in specific situations, but for most healthy individuals, a well-absorbed vitamin D3 supplement is sufficient.
The advantage of calcifediol is that it can reach the bloodstream within just a few hours of taking it.
Blood Levels: The Importance of Getting Tested
The only way to truly know your vitamin D status is through a simple blood test. This test measures the amount of vitamin D circulating in your bloodstream. Knowing your blood levels allows you to determine if you’re deficient, sufficient, or even at risk of toxicity (extremely rare with vitamin D). This information empowers you to work with your doctor to create a personalized plan to reach and maintain optimal vitamin D levels for your unique needs.
